As parents, we all want our children to live long, healthy lives. While there’s no guarantee of reaching centenarian status, there are many evidence-based interventions we can implement to give our kids the best shot at longevity. This guide explores key areas where parents can make a difference, from nutrition and lifestyle choices to disease prevention and safety.
Nutrition: Building Blocks for a Long Life
Whole Foods vs. Processed Foods
A diet rich in whole, unprocessed foods forms the foundation of longevity nutrition. Research has shown that ultra-processed foods are associated with numerous health risks:
- A systematic review found that higher consumption of ultra-processed foods was linked to increased risks of overweight, obesity, abdominal obesity, all-cause mortality, metabolic syndrome, depression, and various cancers[1].
- Ultra-processed food intake was associated with a 62% increased risk of all-cause mortality in a study of nearly 20,000 Spanish university graduates[1].
- A meta-analysis found that higher ultra-processed food intake was associated with increased risk of type 2 diabetes[1].
To promote longevity, encourage your children to eat:
- Fruits and vegetables: Aim for 5 servings daily, focusing on a variety of colors.
- Whole grains: Choose brown rice, whole wheat bread, and oats over refined grains.
- Lean proteins: Include fish, poultry, legumes, and nuts.
- Healthy fats: Incorporate sources of unsaturated fats like avocados, olive oil, and fatty fish.
Foods to Limit or Avoid
Equally important is minimizing foods that can negatively impact health:
- Processed meats: Hot dogs, deli meats, and sausages are high in sodium and preservatives.
- Sugary drinks: Sodas, fruit juices, and sports drinks provide empty calories.
- Artificial sweeteners: These can potentially lead to metabolic issues.
- Fried foods: High in unhealthy fats, they increase heart disease risk.
- High-sugar cereals: Opt for low-sugar, whole-grain alternatives.
The Dangers of Artificial Sweeteners and Fructose
While artificial sweeteners may seem like a healthy alternative to sugar, research suggests otherwise:
- A systematic review found that artificial sweetener consumption was associated with increased risk of type 2 diabetes, cardiovascular disease, and metabolic syndrome[2].
- Frequent consumption of artificial sweeteners may lead to metabolic derangements and, paradoxically, weight gain[2].
Fructose, especially in the form of high-fructose corn syrup, has been linked to various health issues:
- Excessive fructose intake is associated with increased risk of obesity, diabetes, and non-alcoholic fatty liver disease[3].
Preserved Foods and Cancer Risk
Studies, particularly from Asia, have shown associations between preserved foods and cancer risk:
- A meta-analysis found a 52% higher risk of gastric cancer associated with intake of pickled vegetables/foods, with stronger associations in Korea and China[4].
- Consumption of cured meat was significantly associated with increased breast cancer risk in Hong Kong Chinese women[4].
Physical Activity: Moving Towards Longevity
Regular physical activity is crucial for long-term health. The Centers for Disease Control and Prevention (CDC) provides clear guidelines:
- Children and adolescents ages 6 through 17 years should do 60 minutes or more of moderate-to-vigorous physical activity daily[5].
This should include:
- Aerobic activity: Most of the 60 minutes
- Muscle-strengthening: At least 3 days per week
- Bone-strengthening: At least 3 days per week
Encouraging active play, participation in sports, and limiting screen time can help children meet these goals.
Discouraging Illicit Drug Use and Risky Behaviors
Tobacco and Alcohol Prevention
Tobacco use remains a significant health threat to young people. In 2023, 10.0% of middle and high school students reported current use of any tobacco product[6]. To help prevent tobacco use:
- Start conversations early: Begin discussing the dangers of tobacco use when children are 5-7 years old.
- Be a role model: If you smoke, quit. Children of non-smoking parents are less likely to start smoking.
- Establish clear rules: Set firm expectations about not using tobacco and enforce consequences.
- Educate about industry tactics: Teach children to recognize and resist tobacco marketing strategies.
Alcohol remains the most commonly used substance among adolescents. In 2023, about 19.9% of youth ages 14 to 15 reported having at least one drink in their lifetime[6]. To discourage underage drinking:
- Communicate openly: Discuss the risks of alcohol use and your expectations regularly.
- Set a good example: Model responsible alcohol use or abstinence.
- Monitor activities: Know where your children are and who they’re with, especially during teen years.
- Strengthen family bonds: Regular family activities and open communication can reduce the likelihood of substance use.
Preventing Opioid Misuse
The opioid epidemic has had devastating effects on communities across the United States. To help prevent opioid misuse among youth:
- Educate about risks: Discuss the dangers of prescription opioid misuse and illicit opioid use.
- Secure medications: Keep prescription medications, especially opioids, locked away and dispose of unused medications properly.
- Promote alternative pain management: Encourage non-opioid pain management strategies when appropriate.
- Support mental health: Address underlying mental health issues that may contribute to substance use.
Disease Prevention
Cancer Prevention
While not all childhood cancers are preventable, certain strategies can reduce future risk:
- Sun protection: Use sunscreen, protective clothing, and limit sun exposure.
- Healthy diet: Emphasize fruits, vegetables, and whole grains.
- Physical activity: Maintain a healthy weight through regular exercise.
- Vaccinations: Ensure children receive HPV and Hepatitis B vaccines.
- Avoid tobacco exposure: Don’t smoke and avoid secondhand smoke.
Vitamin D and Cancer Risk
Vitamin D has been the subject of numerous studies regarding its potential role in cancer prevention:
- A large clinical trial (VITAL) found that vitamin D supplementation reduced the incidence of advanced (metastatic or fatal) cancer, with the strongest risk reduction seen in individuals with normal weight[7].
- Higher circulating levels of vitamin D (25-hydroxyvitamin D) have been associated with reduced risk of colorectal and bladder cancers[7].
The current evidence suggests that maintaining adequate vitamin D levels may be beneficial for cancer prevention, but more research is needed to establish definitive recommendations. The National Academy of Sciences recommends daily vitamin D intakes of 600 IU for most age groups[7].
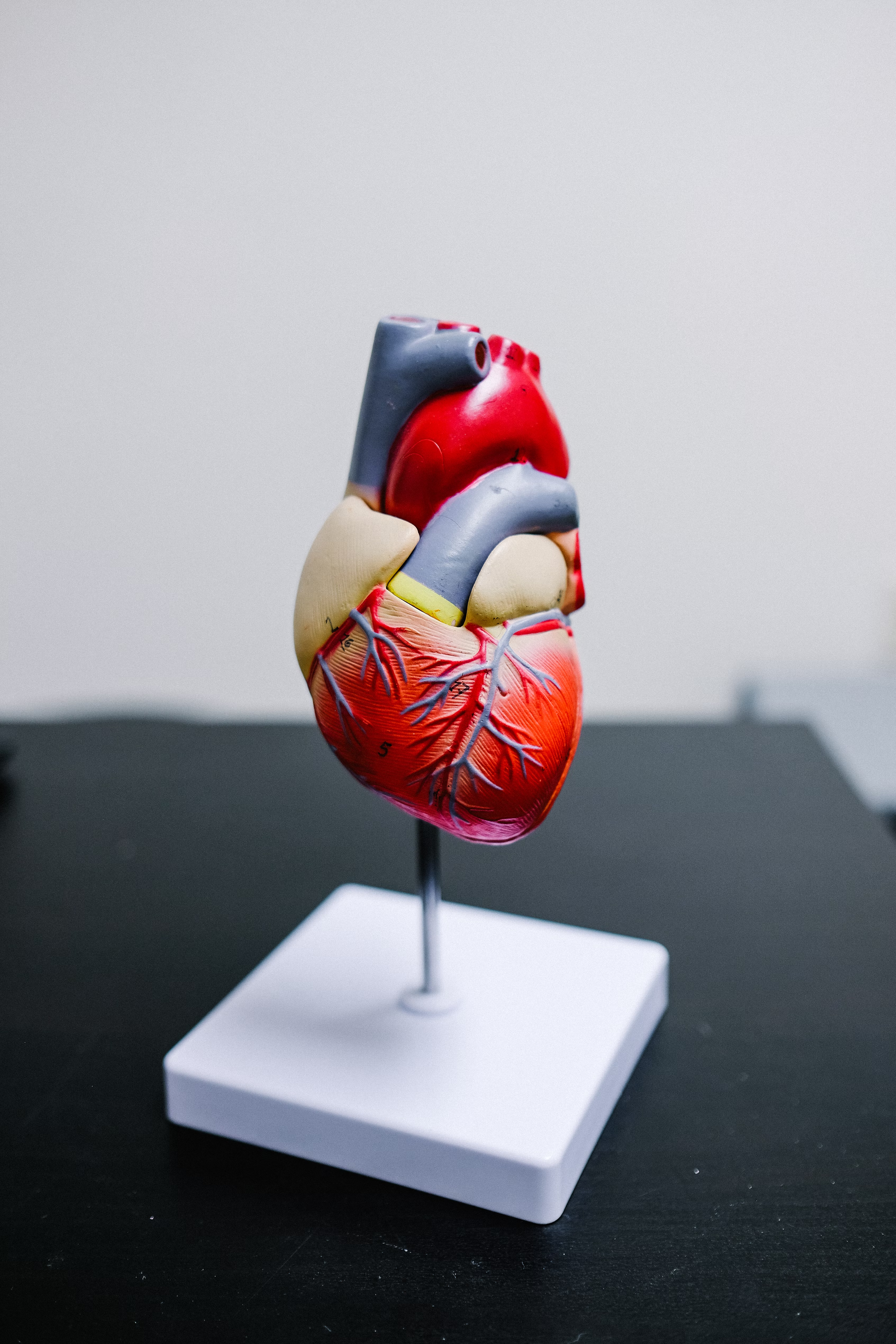
Heart Disease Prevention
Heart health in adulthood starts in childhood:
- Encourage a heart-healthy diet low in saturated fats and high in fruits, vegetables, and whole grains.
- Promote regular physical activity.
- Maintain a healthy weight.
- Monitor blood pressure and cholesterol if there’s a family history of heart disease.
Safety and Accident Prevention
Accidents are a leading cause of childhood mortality. Key safety measures include:
- Use appropriate car seats and teach road safety.
- Childproof your home to prevent falls, poisonings, and choking hazards.
- Teach water safety and ensure proper supervision around water.
- Store medications and household chemicals safely out of reach.
- Ensure proper helmet use for biking and other wheeled activities.
Conclusion
Helping our children live long, healthy lives involves a multifaceted approach encompassing nutrition, physical activity, disease prevention, safety, and overall lifestyle choices. By implementing these evidence-based strategies early in life, we can set our children on a path towards optimal health and longevity.
Remember, it’s never too early to start these healthy habits, but it’s also never too late. Small, consistent changes can make a big difference over time. As parents, we have the power to shape our children’s health trajectories. Let’s use that power wisely to give them the best possible start in life.
Sources
[1] Youth High-Risk Drug Use – CDC https://www.cdc.gov/youth-behavior/risk-behaviors/youth-high-risk-drug-use.html
[2] [PDF] Promising School-based Opioid Prevention Approaches https://www.escneo.org/Downloads/SAMHSA%20Opioid%20Brief.pdf
[3] 6 Ideas for Reducing Risky Behaviors in Teens https://prntexas.org/6-ideas-for-reducing-risky-behaviors-in-teens/
[4] Dietary Recommendations for Healthy Children https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/nutrition-basics/dietary-recommendations-for-healthy-children
[5] Physical Activity Guidelines for School-Aged Children and … https://www.floridanutritioned.org/tip/physical-activity-guidelines-for-school-aged-children-and-adolescents/
[6] Managing Infectious Diseases in Schools – AAP https://www.aap.org/en/patient-care/school-health/managing-infectious-diseases-in-schools/
[7] Evidence-Based Interventions for Preventing Substance Use … https://pmc.ncbi.nlm.nih.gov/articles/PMC2916744/
[8] Invest in Youth Prevention | Opioid Principles https://opioidprinciples.jhsph.edu/invest-in-youth-prevention/
[9] Strategies to Prevent Risk, Promote Health in Teens https://parentandteen.com/coping-strategies-prevent-risk/
[10] Evidence-Based Recommendations and Best Practices for … https://healthyeatingresearch.org/research/evidence-based-recommendations-and-best-practices-for-promoting-healthy-eating-behaviors-in-children-2-to-8-years/
[11] Physical Activity Guidelines for School-Aged Children and … – CDC https://www.cdc.gov/physical-activity-education/guidelines/index.html
[12] Preventing Infectious Diseases | Early Care and Education Portal https://www.cdc.gov/early-care/prevention/index.html
[13] Interventions to Prevent Illicit and Nonmedical Drug Use in Children … https://jamanetwork.com/journals/jama/fullarticle/2766429
[14] Effectiveness of Nutritional Strategies on Improving the Quality of … https://pmc.ncbi.nlm.nih.gov/articles/PMC8781853/
[15] Youth Opioid Prevention – Boys & Girls Clubs of America https://www.bgca.org/get-involved/advocacy/federal-priorities/youth-opioid-prevention/
[16] Preventing Multiple Risky Behaviors Among Adolescents https://www.childtrends.org/publications/preventing-multiple-risky-behaviors-among-adolescents-seven-strategies
[17] Effective Ways to Stop Substance Abuse https://www.schoolcounselor.org/Newsletters/May-2023/Effective-Ways-to-Stop-Substance-Abuse?st=WA
[18] State Strategies for Preventing Substance Use and Overdose … https://nashp.org/state-strategies-for-preventing-substance-use-and-overdose-among-youth-and-adolescents/
[19] [PDF] A Health Promotion Strategy to Preventing Youth Risk Behaviors https://teenpregnancy.acf.hhs.gov/sites/default/files/resource-files/SocialNorms_Denise%20Dickinson.pdf
[20] [PDF] Preventing Drug Use Among Children and Adolescents (Redbook) https://nida.nih.gov/sites/default/files/redbook_0.pdf
[21] Opioid Abuse Prevention – Ohio Department of Education https://education.ohio.gov/Topics/Learning-in-Ohio/Health-Education/Opioid-Abuse-Prevention
[22] Risky behaviour: pre-teens and teenagers – Raising Children Network https://raisingchildren.net.au/teens/behaviour/behaviour-questions-issues/risky-behaviour
[23] Preventing and Reducing Youth and Young Adult Substance Misuse https://www.ed.gov/teaching-and-administration/safe-learning-environments/school-safety-and-security/preventing-and-reducing-youth-and-young-adult-substance-misuse-schools-students-families
[24] Preventing Opioid Use Disorder | Overdose Prevention – CDC https://www.cdc.gov/overdose-prevention/prevention/preventing-opioid-use-disorder.html
[25] Reducing Risk Behavior With Family-Centered Prevention During … https://pmc.ncbi.nlm.nih.gov/articles/PMC6310108/
[26] Tips for Preventing Youth Addiction – Delaware County, Pennsylvania https://www.delcopa.gov/substance/tipsforprevention.html
[27] Preventing risky behaviors among young adolescents in eastern … https://pmc.ncbi.nlm.nih.gov/articles/PMC6261778/
28 Preventing Multiple Risky Behaviors among Adolescents https://www.researchgate.net/publication/265111039_Preventing_Multiple_Risky_Behaviors_among_Adolescents_Seven_Strategies
[29] [PDF] PHYSICAL ACTIVITY IN CHILDREN AND ADOLESCENTS https://www.acsm.org/docs/default-source/files-for-resource-library/physical-activity-in-children-and-adolescents.pdf
[30] Disease Prevention and Health Promotion | City of Berkeley https://berkeleyca.gov/safety-health/public-health/disease-prevention-and-health-promotion
[31] Effectiveness of Nutritional Strategies on Improving the Quality of … https://pubmed.ncbi.nlm.nih.gov/35057552/
[32] Physical activity guidelines for children and young people – NHS https://www.nhs.uk/live-well/exercise/physical-activity-guidelines-children-and-young-people/
[33] Everyday Actions for Schools to Prevent and Control the Spread of … https://www.cdc.gov/orr/school-preparedness/infection-prevention/actions.html
[34] How to teach kids healthy eating habits: Dietitian’s 10 tips https://engagement.source.colostate.edu/research-based-tips-mealtime-success-kids/
[35] [PDF] Physical Activity Guidelines for Americans, 2nd edition https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf
[36] Prevention of noncommunicable diseases https://www.who.int/teams/maternal-newborn-child-adolescent-health-and-ageing/child-health/prevention-of-noncommunicable-diseases
[37] Nutrition for kids: Guidelines for a healthy diet – Mayo Clinic https://www.mayoclinic.org/healthy-lifestyle/childrens-health/in-depth/nutrition-for-kids/art-20049335
[38] 2020 WHO guidelines on physical activity and sedentary behaviour … https://pmc.ncbi.nlm.nih.gov/articles/PMC7691077/
[39] Protecting Your Child From Infections – MyHealth Alberta https://myhealth.alberta.ca/Health/pages/conditions.aspx?hwid=ue5130
[40] American Heart Association Recommendations for Physical Activity … https://www.heart.org/en/healthy-living/fitness/fitness-basics/aha-recs-for-physical-activity-in-kids-infographic
[41] Children – Healthy People 2030 | odphp.health.gov https://odphp.health.gov/healthypeople/objectives-and-data/browse-objectives/children
[42] Child Activity: An Overview | Physical Activity Basics – CDC https://www.cdc.gov/physical-activity-basics/media/images/Kidsrunning169.jpg?sa=X&ved=2ahUKEwiVzqGFv-6KAxX7G9AFHW6jHkYQ_B16BAgDEAI
[43] Reducing the Spread of Illness in Child Care – HealthyChildren.org https://www.healthychildren.org/English/health-issues/conditions/prevention/Pages/Prevention-In-Child-Care-or-School.aspx